|
When you are trying to achieve an optimal weight, it becomes even more important to eat the correct foods. Most people have a definite awareness of foods that may contribute to weight gain. Although carbohydrates have been vilified, it is important to judge carbohydrates according to their nutritional value. In general whole grains and vegetable carbohydrates are part of a healthy balanced diet. Whole Grains include foods like brown and wild rice, quinoa, buckwheat, teff, oats, rye, organic corn, spelt and millet. All vegetables are part of a healthy diet, except for potatoes that are high on the glycemic index and not good for blood sugar balance. Most of our carbohydrates should be obtained from veggies.
Every balanced meal should also include proteins and healthy fats. Examples of good proteins are chicken, fish, low fat dairy, eggs, beef and seafood, preferably from an organic source. Examples of good fats are avocados, healthy oils like avocado, olive or nut oils, nuts and seeds, fish and coconut oil/milk. As said before every meal should include a protein, fat, protein and complex carbohydrates. A carbohydrate should never be eaten alone, always in combination with a protein. Doing this will ensure that blood sugar levels remain stable. Weight loss can only be achieved if blood sugar levels are stable. Another common obstacle to weight loss is a "too long" feeding period. The body needs a break to process the glucose in the system and body cells. You might have heard of intermittent fasting and the advantages of it in weight loss. A 16 to 18 hours break in eating after dinner has been proven in studies to be beneficial for weight loss. This means that if you eat dinner at 7, that your fast should only be broken at 11am or 12am respectively. Over a period of time implementing intermittent fasting, the body will become more sensitized to insulin and achieving a healthy blood sugar balance becomes the norm. This will then be very favourable for weight loss. All of this might seem daunting and you are thinking that you are going to be starving to death with all these changes. On the contrary, the amount of food that you eat per serving is not the biggest concern, the type of foods as well as when you eat still remains of more importance. Like any new habit, the change to healthy foods will begin gradually and in no time you will feel equipped in stocking your fridge and cupboards with different foods as well as preparing different foods for meals. Eating a healthy diet is an important factor when you want to achieve an optimal and healthy body weight. Please contact the Naturopathic health care centre for more guidance with weight loss. Dr Marike de Klerk Homeopath
0 Comments
Different types of tapes were covered: Dynamic tape, Kinesiology tape, McConnell tape, and Athletic tape.
Dynamic tape A biomechanical tape that helps with function, manages load, and can modify movement patterns. Kinesiology tape Kinesiology tape promotes lymphatic and blood circulation and reduces pain sensitivity. McConnell tape Affects biomechanics and is mainly used for rehabilitation. Athletic tape Athletic tape is used for injury prevention, and is usually worn for a short amount of time. Endometriosis can be debilitating, especially during a flare up. The severe pain can disrupt your daily life and limit your activities. This affects your quality of life and can be emotionally very challenging.
What causes these flare ups? It could be one of these; hormonal fluctuations, stress, increased inflammation, or fatigue. Tracking these triggers and an awareness can help you to avoid and manage them with a game plan. An aggravation episode can be explained as a time in your cycle where symptoms are more pronounced. Endometriosis is a disease where some endometrial lining outside the uterus responds to your monthly hormonal fluctuations. This process of thickening and elimination of the lining can cause the inflammation and pain experienced. The following are symptoms of endometriosis:
The intensity of these flare ups are dependant upon many factors and what is happening in your body. These are some of the triggers:
Stress increases cortisol levels. This will increase inflammation in the body, potentially aggravating endometriosis symptoms. Chronic stress can also affect hormones in other ways, such as by decreasing estrogen or progesterone, and therefore causing endometriosis or aggravating this condition. Foods that can contribute to gut dysfunction and inflammation are processed foods, red meat, dairy products, and foods high in trans fats or refined sugars. Poor diet can aggravate endometriosis. It is essential to have a nutrient dense rich diet dominated by anti inflammatory antioxidant rich foods. Just as bad as inactivity, too much exercise or lots of physical activities that put pressure on the pelvic region, such as high-impact workouts or intercourse, can sometimes trigger a flare-up of your endometriosis. A balance between good and bad bacteria in your digestive tract is essential for immune response and regulating inflammation. The bacteria in your intestines are also very important regulators of all hormones. Dysbiosis is thought to worsen endometriosis and to cause flare ups. A poor diet, stress and infections treated with antibiotics or cortisone can worsen gut function. Medications containing estrogen can stimulate the growth of the endometrial tissue in areas outside of the uterus. These drugs could be oral contraceptive pills, hormone replacement therapy, and fertility drugs. The following supplements may be beneficial in the management of endometriosis
Living with endometriosis often means facing very uncomfortable flare-ups that can impact your daily life, such as intense pain, bloating, and fatigue. By identifying personal triggers and implementing effective relief strategies, you can achieve better symptom control and overall well-being. To better manage endo flare-ups, consider keeping a diary to track the effects of your diet, exercise routine, stress levels, and use of medications. Remember, you don't have to suffer in silence—seek support from knowledgeable healthcare professionals who can offer valuable guidance and resources tailored to your unique needs. by Dr. Marike de Klerk
As many as 50 % of women have hair loss in their menopausal years. The type of hair loss in menopause is defined as female pattern hairloss. This occurs when the size of hair follicles decreases, causing hair thinning and fewer hairs on the head. Female pattern hairloss mostly affects the central scalp and can be noticed along the part line, the front hair line, and the sides of the hair. It may also come out in clumps while showering or brushing your hair. In addition to the hair shaft reducing in thickness, the growth phase may be affected and more hair breakage may occur. Female hair loss in menopause has many causes and can include the hormonal influence on hair follicles, genetics, stress, and nutrient deficiencies. Studies suggest that hormone imbalances that occur in menopause, primarily a change in estrogen and progesterone can be to blame. Estrogen and progesterone declines in late perimenopause and into the postmenopausal years and hair growth is slowed. These two hormones are very important for healthy hair growth and without them, the hair can become thin, dry, and break easily. Estrogen is an essential hormone for overall healthy skin. Estrogen helps keep the skin firm, plump, and hydrated. When estrogen levels decline with menopause, it accelerates skin aging and also affects the hair follicles and can contribute to hair loss and thinning. When the body is actively converting estrogen to testosterone during menopause, this reduces the follicle's exposure to androgens. In some cases, the production of androgens or male hormones, including testosterone, can lead to shrinking of the hair follicle and hair loss. When high androgen is the issue, women experience hair loss on the head and can also see hair growth on the chin or upper lip. Progesterone is produced by the ovaries after ovulation, but as ovulation stops, the levels of progesterone decline. Progesterone also blocks the production of excess testosterone and prevent it from being converted into its stronger form, dihydrotestosterone or DHT. DHT is largely responsible for changes to the hair follicle that result in hair loss and thinning. Hypothyroidism and hyperthyroidism can both result in hair loss.The decline in estrogen and progesterone with menopause slows metabolism. It’s common for women to gain some weight in menopause, and an increased weight correlates with female hair loss . Insulin and blood sugar can also play a role in hair loss. It is important to try and identify the reason for this hairloss and adressing it in a effective way. Sister Alida Idema
It is found in the root of the nose. Think aeroplane cabin…. Back in the 1930’s the first aircraft was equipped with a pressurised cabin, enabling passengers and crew to breath more comfortably in the thinner air when reaching high altitudes. Since then, cabin pressurisation has become a technology that most passengers take for granted. Cabins are pressurised by pumping fresh air into them after which the air is cooled and humidified and then circulated throughout the cabin. Apart from creating a more comfortable environment, it is an important safety feature. Your cells need oxygen to produce energy and help your organs and tissues to do their jobs. Iron, that is contained in the haemoglobin of the blood, carries oxygen to every cell in the body. So, once the cabin achieves an ideal pressure level that is safe for the passengers, the aircraft maintains it at that level. However, sometimes things go wrong for whatever reason, As the aircraft cabin loses its pressure, oxygen masks will automatically drop down in front of passengers. Normally our bodies can maintain optimal oxygen levels enabling all our systems to work properly, but sometimes we need to supplement with the oxygen carrier, Ferrum phos. Ferrum phos is known as the first aid remedy and is the most important tissue salt to take at the first sign of infection and inflammation. It brings oxygen to the cells that assists healing. It is able to strengthen the blood vessels and their ability to distribute oxygen rich blood to the cells and carry the carbon dioxide back to the lungs. The presence of Ferrum phos activates all sort of processes within the body especially the process of releasing energy from the food we eat. Chronic conditions that ask for supplementing with Ferrum phos are fatigue and exhaustion, poor concentration, low immune resistance, migraines and headaches, rheumatoid pains. In acute cases Ferrum phos is given during the first stages of a common cold, earache, sore throat, feverish conditions (with pulsating pain, flushed cheeks and ears), joint pains, red and burning eyes, menstrual pain and gastrointestinal conditions. Foods that are rich in ferrum phos are garlic, celery, parsley, spinach, radishes and lettuce. Our hard-working bodies and busy minds can benefit by eating lots of these, fresh or cooked. And finally, take Ferrum phos - tissue salt no. 4 every day. Perimenopause and your thyroid.
Perimenopause is the phase before menopause. It can begin as early as in your thirties, but usually start between ages 40 and 45. You might start noticing that your period is changing- it might be longer or shorter, more frequent or skipping cycles, more or less flow, as well as symptoms that comes with hormonal changes. Perimenopause can last a few months upto a few years. Once you have had no period for 12 months, the perimenopausal phase is complete and menopause has started. Some women struggle more than others during perimenopause. Troublesome symptoms may include hot flashes, irregular periods, breast tenderness, fibrocystic or lumpy breasts and decreased libido. These symptoms are often like the ones you suffered from when you had PMS. Less obvious symptoms that seem unrelated to the female system can also be related to hormonal imbalances such as weight gain/increased fat storage (especially in the thighs, hips, and breasts), water retention, fatigue, brain fog, sleep difficulties, mood swings, insomnia, headaches, hair loss, and joint pain. Women are very likely to develop a thyroid condition during perimenopause, or experience a worsening of thyroid symptoms, because of the hormonal changes that are happening during this time. Oestrogen dominance is the main culprit in causing perimenopausal and thyroid symptoms. Although oestrogen and progesterone both decline during perimenopause, progesterone declines at a much faster rate, therefore causing progesterone to be lower in comparison to oestrogen, called relative oestrogen dominance. In a nutshell, this means that sometimes a woman may have normal progesterone, but may have symptoms of progesterone deficiency due to a hormonal imbalance caused by estrogen levels that are too high. Other times, women are symptomatic due to unopposed estrogen relative to progesterone, meaning that they have normal estrogen and low progesterone. If you have estrogen dominance, your conversion from T4 to T3 will not be optimal, leading to thyroid symptoms. Everyday events that can contribute to the increased levels of oetrogen are oral contraception pills, decreased detoxification, estrogen-mimicking toxins (also called xenoestrogens), gut issues, stress, and thyroid conditions. Low Progesterone SymptomsProgesterone is called "the happy hormone" and plays an important role in our mood, sleep, and bone health. It is also important for fertility. It is helpfull in reducing hot flushes and night sweats. Low progesterone leads to low thyroid levels. Here are some common symptoms of low progesterone:
The following supplements and advice can be used to boost progesterone naturally:
Progesterone is an important hormone during our fertile and childbearing years, but don't neglect your progesterone at any time during your lifeline as it will always play an important role in many bodily functions, not just for thyroid health. Dr Marike de Klerk Constipation can cause a decline in your brain function.
We all know by now how important our gut function is for overall health, but the link between gut function and brain function decline is not that well known yet. Studies done recently are revealing that there is a very probable link between poor gut health, especially chronic constipation and early dementia. Chronic constipation may not only be a red flag for poor gut health, but a potential warning sign of cognitive decline. Researchers found that among more than 110,000 middle-aged and older adults, the ones who were chronically constipated, having fewer than three bowel movements a week, showed early signs of poor brain health. The findings presented at a meeting of the Alzheimer's Association in Amsterdam showed that people with chronic constipation typically performed worse on tests of memory and thinking. In addition, 73% of these same people reported that they were concerned about a decline in their cognitive function. The theory behind this research is that constipation and cognition are linked via the gut microbiome. The science is exploding with research linking abnormal gut microbiome and various diseases, including degenerative brain diseases like Alzheimer's. Constipated patients with cognitive decline tended to have relatively few gut bacteria that produced butyrate, an important fatty acid that helps control inflammation. If your brain capacity has become a concern to you, or perhaps your parents are showing signs of accelerated decline in brain function, please consider addressing their gut function. If they are constipated, this becomes a priority to be sorted out. Always remember there are much more to be rectified in the gastrointestinal tract than just replacing good bacteria. The gut functions as an "orchestra" and every musical instrument need to play "in tune" for the melody to be beautifull. Dr. M de Klerk Chiropractic treatment is a non-invasive form of healthcare that aims to improve musculoskeletal function and alleviate pain. This approach is based on the belief that the body has the ability to heal itself, and that by removing any interference in the nervous system and improving mobility the body can function optimally.
Chiropractors use a variety of techniques to treat pain and improve the function of the musculoskeletal system, including joint manipulation, soft tissue therapies, and exercise recommendations. In this article, we will explore how chiropractic treatment improves pain and affects pain pathology. What is pain? Pain is a complex phenomenon that is influenced by both physical and psychological factors. It is a protective mechanism that signals the presence of tissue damage or injury and is essential for survival. However, chronic pain can be debilitating and have a significant impact on a person’s quality of life. It is estimated that chronic pain affects approximately 1 in 5 people in South Africa alone. Chiropractic treatment is one of the many approaches used to manage chronic pain, and it has been shown to be effective in reducing pain and improving function in many patients. How do Chiropractors treat pain? Chiropractors use a variety of techniques to treat pain, including joint manipulation, soft tissue therapies, and exercise recommendations. Joint manipulation involves the application of a controlled force to a joint to restore proper function, and yes chiropractors can treat any joint not just the spine. This technique is based on the belief that misalignments in the spine (subluxations) can interfere with the nervous system and lead to pain and dysfunction. By correcting these subluxations, chiropractors aim to improve nerve function, mobility and reduce pain. Soft tissue therapies are another important component of chiropractic treatment. These therapies include massage, myofascial release, and trigger point therapy. Soft tissue therapies aim to relieve muscle tension and improve circulation, which can help to reduce pain and improve function. In addition to joint manipulations and soft tissue therapies, chiropractors also provide exercise recommendations to help patients improve their strength and flexibility. These exercises are tailored to the individual patient’s needs and are designed to support the body’s natural healing process. How effective is chiropractic treatment in managing pain? The effectiveness of chiropractic treatment in managing pain has been studied extensively, and the results are promising. A systematic review of 26 randomized controlled trials found that chiropractic care is effective in reducing pain in patients with low back pain, neck pain, and shoulder pain. Another systematic review of 32 randomized controlled trials found that chiropractic care is effective in improving function in patients with low back pain, neck pain, and headaches. In conclusion Chiropractic treatment has shown to affect the nervous system, including the sympathetic nervous system and the hypothalamic-pituitary-adrenal axis. These systems play a role in the body’s response to stress and pain, and by modulating their activity, chiropractic treatment may help to reduce pain and promote healing. In short chiropractic treatment improves pain by reducing inflammation, improving circulation, and restoring proper joint function. Exercise recommendations may also help to improve muscle strength and flexibility, which can reduce the risk of future injuries and pain. Chronic pain is a debilitating condition that affects millions of people worldwide. It is characterized by persistent pain that lasts for more than three months and often does not respond to conventional pain management techniques.
Chronic pain can have a significant impact on a person’s quality of life and can lead to depression, anxiety, and other mental health problems. Understanding the complex mechanisms involved in chronic pain is crucial in developing effective treatments for this condition. In this article, we will explore the process of chronic pain, including the neurotransmitters and cytokines involved. The Process of Chronic Pain Chronic pain is a complex process that involves the nervous system, the immune system, and the brain. It is caused by a variety of factors, including injury, inflammation, and nerve damage. In the case of chronic pain, the pain signals persist even after the initial cause of the pain has been resolved. When an injury occurs, pain signals are sent to the brain through the nervous system. These signals are transmitted by neurotransmitters, which are chemicals that allow nerve cells to communicate with each other. Some of the neurotransmitters involved in chronic pain include substance P, glutamate, and GABA. Substance P is a neuropeptide that is involved in transmitting pain signals to the brain. It is released by sensory neurons in response to injury or inflammation. Glutamate is an excitatory neurotransmitter that is involved in the transmission of pain signals in the spinal cord. GABA is an inhibitory neurotransmitter that helps to regulate pain signals in the nervous system. In addition to neurotransmitters, cytokines also play a role in chronic pain. Cytokines are proteins that are produced by immune cells in response to injury or inflammation. They help to regulate the immune response and are involved in the development of chronic pain. Some of the cytokines involved in chronic pain include TNF-alpha, IL-1 beta, and IL-6. TNF-alpha is a pro-inflammatory cytokine that is involved in the development of neuropathic pain. IL-1 beta is a cytokine that is released by immune cells in response to injury or infection. It is involved in the development of chronic pain by sensitizing pain receptors in the nervous system. IL-6 is a cytokine that is involved in the development of chronic pain by increasing the production of substance P and other pain-related neurotransmitters. The Role of the Brain in Chronic Pain The brain also plays a crucial role in chronic pain. When pain signals are transmitted to the brain, they are processed in the somatosensory cortex, which is responsible for processing sensory information. The brain also has areas that are involved in emotional and cognitive processing, which can influence the experience of pain. The limbic system, which is involved in emotional processing, can amplify or diminish the experience of pain. The prefrontal cortex, which is involved in cognitive processing, can also influence the experience of pain by modulating attention and expectation. Conclusion Chronic pain is a complex process that involves the nervous system, the immune system, and the brain. It is caused by a variety of factors, including injury, inflammation, and nerve damage. Chiropractors use a variety of techniques to treat and improve the function of the musculoskeletal system, including spinal adjustment, soft tissue therapies and exercise recommendations. Dr. Marlo also makes use of various homeopathic, herbal and supplemental remedies to alter pain pathways in order to improve and manage pain. Last week, 3 years ago, our president declared a disaster state and locked us down for 21 days. Many people contracted COVID, some of them tragically passed away. Some patients recovered completely from the infection with no lasting symptoms.
Unfortunately, others suffered and are still suffering from what we call long COVID syndrome. At least 17 million people in the WHO European region experienced long COVID in the first two years of the pandemic; millions may have to live it for years to come. Many of the “long haulers” experiences heart symptoms like palpitations, dizziness, chest pain, shortness of breath, tightness of chest, tachycardia, and blood pressure regulation problems. Why did these patients’ hearts get affected and damaged? Temporary or lasting damage to heart tissue was due to several factors: Lack of oxygen. As the virus caused inflammation and fluid to fill up the air sacs in the lungs, less oxygen reached the bloodstream. The heart had to work harder to pump blood through the body, which was especially dangerous in people with pre-existing heart disease. Some hearts failed from overwork, or insufficient oxygen that caused cell death and tissue damage in the heart and other organs. Myocarditis: inflammation of the heart. The coronavirus infected and damaged the heart’s muscle tissue directly, as is possible with other viral infections, including some strains of the flu. The heart also became damaged and inflamed indirectly by the body’s own immune system response, called the cytokine storm. Coronavirus infection also affected the inner surfaces of veins and arteries, which caused blood vessel inflammation, damaged small vessels and blood clots, all of which compromised blood flow to the heart or other parts of the body. Stress cardiomyopathy. COVID infection also caused cardiomyopathy, a heart muscle disorder that affected the heart’s ability to pump blood effectively. When the virus attacked, the body underwent stress and released a surge of chemicals called catecholamines, which stunned the heart. Most serious of all, was the immune system that launched an attack on the invading virus that was so severe that it destroyed healthy tissues. When responding to infection with the coronavirus, the body released a flood of proteins called cytokines that helped cells communicate with one another and fight the invaders. In some people, perhaps due to a genetic difference, this normal defensive event was exaggerated, leaving them vulnerable to a cytokine storm. In this cytokine storm, the immune system response causes inflammation that overwhelmed the body, destroying healthy tissue and damaging organs such as the kidneys, liver and heart. The cytokine storm and its resulting heart damage also affected the heart’s rhythm. Serious ventricular arrhythmias due to a cytokine storm was for some patients catastrophic. The cytokine storm was difficult to survive. The damage for this immune reaction is a complicated problem and is probably the cause of residual inflammation in the cardiovascular system that cause long- haul COVID cardiac symptoms. There are currently treatments that can improve and hopefully in the long-term cure this conditions. As time goes on, I am sure more therapies will come to light. For now, it is a relief to know that we need not be despondent about this conditions, since alternative and functional remedies and medicines can assist favourably. Often the body just needs assistance to heal and bring the body back into homeostasis. For more information on how we can assist you, please contact the practice on 012 460 9216. Heart Rate and COVID-19 After you have had COVID-19, if you are experiencing a rapid heartbeat or palpitations, you should contact your doctor. A temporary increase in heart rate can be caused by a lot of different things, including dehydration. Make sure you are drinking enough fluids, especially if you have a fever. Symptoms of a rapid or irregular heart rhythm may include:
How can I tell if I have developed a heart problem after COVID-19? In some people, heart rates can vary from fast to slow, unrelated to exertion, for no apparent reason. But, Post says, shortness of breath, chest pain or palpitations after having COVID-19 is a common complaint. “Any of these problems could be related to the heart, but they could also be due to other factors, including the aftermath of being very ill, prolonged inactivity and spending weeks convalescing in bed.” Shortness of Breath “You want to consult a doctor if any of your symptoms are severe, especially shortness of breath,” Post says. She recommends using a commercially available O2 (oxygen) saturation monitor. “Shortness of breath by itself is not always a sign of a serious problem, but if you have that symptom along with low O2 (below 92%), that is a reason to be concerned.” Sometimes people are short of breath with exertion after COVID-19 because they have been less active for a long time and need to gradually build their fitness level back up. A diagnosis of heart failure after COVID-19 is rare. But if you have shortness of breath or leg swelling after COVID-19, you should contact your doctor, who may recommend evaluation by a cardiologist if tests indicate you are at risk. COVID-19 Chest Pain What about lingering chest pain, another common post-COVID complaint? “Chest pain may be nothing serious, but if you are having severe chest pain, get help, especially if it is persistent or if you are also having nausea, shortness of breath or lightheadedness: These could be symptoms of a heart attack.” “If you have chest pain when you inhale, you might have lung inflammation. Sudden, severe chest pain could be a blood clot in the lung (pulmonary embolism),” Post says. People recovering from the coronavirus sometimes show symptoms of a condition known as POTS (postural orthostatic tachycardia syndrome). Researchers are exploring whether or not there is a link. POTS isn’t directly a cardiac problem, but a neurologic one that affects the part of the nervous system that regulates heart rate and blood flow. The syndrome can cause rapid heartbeats when you stand up, which can lead to brain fog, fatigue, palpitations, lightheadedness and other symptoms. Can COVID-19 symptoms mimic a heart attack? Yes. People with COVID-19 can have symptoms similar to those of a heart attack, including chest pain, shortness of breath and changes on their echocardiogram (ultrasound of the heart) or EKG. But often when these patients are given an angiogram, there is no evidence of a major blockage in the heart’s blood vessels, which would indicate a heart attack in progress. Symptoms of myocarditis can also mimic those of a heart attack. Also, viral infections such as COVID-19 can cause very small blood clots to form, which can block tiny blood vessels and cause pain. People with signs and symptoms of a heart attack should seek urgent medical attention and not manage these symptoms at home. It is found in the bones.
Think Kreepy Krauly… That magic pool cleaner that works day and night, clearing away all the decaying matter from the floor, climbing up the steps and suctioning off the accumulating dirt and debris from the sides. It removes all the waste by washing it through a filter system and circulating the purified water back to your pool. Without a proper cleaning system this material may otherwise lay dormant and decay slowly, causing damage to the surroundings and an irregular pH for the water. In the end, not only the water, but the marbelite and all other structures will be in a total mess, and nobody will want to use the pool anymore. Wouldn’t it be nice if we had such a thing in our bodies? The digestive system is forever working to chew, mash, digest, and reject what comes in through the mouth. So does the liver, gall, kidneys, and the urinary system. The same happens in the respiratory system. Whatever we breath in needs to be made useful or rejected. Another example is our vascular and lymphatic system. Our skin, the largest organ in the body is constantly getting rid of fluids filled with toxins, salts, and puss. Like the vacuum pool cleaner, these systems all work together to maintain a perfect balance in our bodies, preventing it to become such a mess, that we do not want to use it anymore. The Calc Sulph found in our bones assist in destroying old cells, abnormal discharges of puss, mucous and catarrh. However, sometimes things go wrong, and our systems fail. You might pick up a bad bug, anything from an ordinary cold to a stomach bug or a septic wound. You might battle with acne and pimples, boils, or slow healing ulcers. Suppurating insect bites, conjunctivitis (pink eyes) or another type of yellow discharge from the eyes. Other symptoms may be built up earwax, bleeding gums and mouth ulcers, tonsillitis, nasal discharge, and productive coughing. Furthermore, insomnia, general irritation and headaches could all be as a result of toxins in the blood from becoming liverish. That is when you need to supplement with Calc Sulph. Foods that are rich in calc sulph are onions, garlic, leeks, cauliflower, figs, prunes, celery, and parsley. These suffering bodies can benefit by eating lots of these, fresh or cooked. And finally, take Calc Sulph - tissue salt no. 3 every day. Article by Sister A Idema Dr. M de Klerk
Recurring cystitis can be a frustrating, debilitating condition that can interfere with daily life and sometimes even relationships. Cystitis is the term used for the inflammation of the bladder, and this inflammation is most commonly caused by a bladder infection. Some people are naturally just more prone to developing cystitis without any real cause. However, there are also a number of more specific causes that you should look out for, as knowing the cause makes it easier to prevent. 1. Not fully recovering from a previous infection As soon as the burning sensation and constant need to pee disappears we relax on the cranberry juice, or our water intake drops right down and we think we can get back to our usual routines. However, this can be a bit hasty, as at this point there may still be some bacteria left in the bladder that can quickly begin to multiply again if you aren’t carefull. Many natural products including homeopathic medicines as well as herbals can be used to make sure that the infection is cleared entirely. Please contact Naturopathic health care centre for advice on treatments. 2. Disruption to intimate or gut floraOur bodies are naturally home to a whole host of bacteria, and usually our friendly bacteria have the important responsibility of helping to keep our bad bacteria in check. However, things like antibiotics, poor diet or an over-use of antibacterial soap can easily alter this balance, and leave bad bacteria free to multiply. Specific strains of bacteria as well as certain foods can promote a diversity of good bacteria in your genitourinary tract and protect you from invaders that can cause disease. 3. Poor immune functionsIf your cystitis or UTIs follow the pattern of repeat infections, then it might be that your immune system isn’t working to its maximum potential. You rely heavily on your immune system to detect and eradicate any infection, be it located within your urinary tract or elsewhere. Herbals as well as homeopathic medicines can be used to enhance our inherent immune system. Contact Naturopathic health care centre for advice. - Dr. Marlo Swanepoel
A muscle cramp is a sudden and involuntary contraction of one or more of your muscles. Though generally harmless, muscle cramps can make it temporarily impossible to use the affected muscle. They are extremely common, particularly in the legs, feet and hands and at times the abdomen and ribcage. Generally, a cramp can last from a few seconds to minutes. Long periods of exercise or physical activity, particularly in hot weather, can lead to muscle cramps. They may affect any age and may also occur at rest. Causes of muscle cramps may be classified as: o Physiologic - Dehydration causing electrolyte imbalance - Overuse - Nocturnal (night cramps) - Pregnancy o Metabolic - Malnutrition – Deficiencies in B vitamins., magnesium, calcium and vitamin D - Underactive thyroid gland - Liver disease - Kidney disease o Medicine induced - Diuretics - Statins o Pathologic - Various neurological conditions and myopathic including stroke, Parkinson’s etc Why cramps occur is not always clear and the cause is not always clearly understood. Some theories of muscle cramps include: o Electrolyte disturbances affecting the contraction and relaxation of muscles, caused by exercise, overuse or some medication o Neural fatigue caused by overuse o Neurological disorders causing hyperexcitability of the nerves innervating the muscles. o Inadequate circulation causing a lack of oxygen and nutrients and a build-up of metabolic waste products. o Nerve root compression Treatment strategies o Ensure adequate fluid and electrolyte intake o Ensure adequate mineral intake o Ensure proper acid-alkaline balance o Stimulate peripheral circulation Diet strategies to improve and prevent cramps o Unrefined sea salt o Potassium: found in fruit and vegetables, especially bananas, sweet potatoes, avocadoes, green leafy vegetables, nuts and seeds etc o Calcium: dairy foods, nuts and seeds, green leafy vegetables o Magnesium: green leafy vegetables, whole grains, nuts and seeds, legumes, raw cacao Supplements that support Muscle Cramps o Magnesium – ensure that calcium to magnesium ratio does not exceed 2:1 esp if takin calcium supplements o Potassium o CoQ10 – especially if using statin medication o L-Arginine – vasodilator, be cautious is on blood pressure medication or if you suffer from low blood pressure Herbal support o Spasmolytic – ginger, crampbark, valerian o Circulatory stimulant, peripheral vasodilator – 78ginkgo, ginseng Physical measures o At first sign of cramp, stop and stretch muscle o Apply heat to cramping muscles o Ensure adequate fluid and electrolyte replacement when exercising If your muscle cramps are chronic or excessive related to the level of activity or do not resolve with the common treatment methods then further investigation by a health care professional is required. -By Dr. Marlo Swanepoel
Diabetes mellitus (aka sugar diabetes as called by many south Africans) is a metabolic disorder in which the body becomes resistant to the effect of insulin or where the body does not produce enough of insulin. Therefore, there is a build-up of glucose (sugar), in the body. This excess glucose can lead to serious health complications. During 2016 and 2017, Diabetes was the second leading underlying cause of death in South Africa and the number one cause of death in females. It was estimated that 4.58 million people between the ages 20 and 79 years old suffered with diabetes in South Africa in 2019. There was a rapid increase in the prevalence of diabetes, from 4.5% in 2010 to 12.7% in 2019. This caused South Africa to be named the unhealthiest county in the world in 2019. This in turn lead to the sugar tax being implemented and increased by the South African Government in order to fight the global Diabetes pandemic. Types of Diabetes Mellitus There are two main types of Diabetes Mellitus:
Testing for Diabetes Doctors will do a blood test to measure HbA1C levels. This stands for glycated haemoglobin. This test measures how well the body controls glucose over a period of 120 days, which is the lifespan of a red blood cell. Red blood cells contain haemoglobin. This protein is responsible for carrying oxygen. Once haemoglobin binds to glucose it becomes glycated. The higher the blood glucose levels the higher the number of glycated red blood cells would be thus the higher the HbA1C level. Normal HbA1C levels should be less than 5.7%. People are diagnosed with Diabetes if their HbA1C levels are higher than 6.5%. Complications of Diabetes
Prevention of Type 2 Diabetes Mellites Progressing from prediabetes to diabetes isn’t certain. Some risk factors like age, sex and genetics may not be altered but this does not mean it will cause or lead to diabetes. As mentioned before Type 2 Diabetes is mainly caused by lifestyle. How to reduce the risk
If you missed it, herewith a recording of my talk with Dr. Hema Kalan about acute childhood illnesses. Dr. Marike de Klerk Pomegranate is called the jewel of the fruits, not only because the seeds look like small gems, but also because of all the incredible health benefits.
- Antioxidant- it is rich in polyphenols that reduces the free radicals that can damage the body. - Nutrient boost- it contains an abundance of Vit E, Vit C, Vit K and magnesium. -Cancer prevention- polyphenols prevents the growth of cancer cells especially in the prostate, liver, lungs and skin. -Alzheimers- prevents the formation of amyloid plaques in the hippocampus. - Digestion- it reduces inflammation in IBD. - Inflammatory conditions- it reduces inflammation . - Arthritis- acts as an anti inflammatory and antioxidant. - Heart- it reduces systolic blood pressure and protects heart and arteries. -Antimicrobial - anti viral and anti bacterial activity - Memory- it improves learning and memory - Endurance and sport performance- it increases performance and post recovery rate. - Sexual performance and fertility- helps with spermatic dysfunction and increases mobility of the sperm - Wound healing- external application New research suggests constant bitterness can make you ill.
What is bitterness? It is anger, resentment, and disappointment at being treated unfairly. Bitterness can be based on one incident or life circumstances. According to psychologist Dr. Carsten Wrosch, persistent bitterness, when strong enough could affect your health. “When harbored for a long time,” Wrosch said, “bitterness may forecast patterns of biological dysregulation (a physiological impairment that can affect metabolism, immune response or organ function) and physical disease.” “In order to deal with bitter emotions there is something required to enable a person to overcome the negative emotion — that something is forgiveness,” said Wrosch. The first step to overcoming bitterness is to have forgiveness. Some people have definitely experienced some profound events in their life and have every reason to be bitter. However, this emotion does not hurt your offender. It only hurts you. When you forgive, the offending person or situation no longer has power in your life. Bitterness and associated diseases There is evidence to show that suppressed anger (bitterness) can be a stimulant to the development of cancer, and also a factor in the progression of the cancer after diagnosis. Anger (bitterness) frequently accompanies autoimmune diseases. Proneness to anger (bitterness) places middle-aged men and women at significant risk for Coronary Heart Disease. Anger (bitterness) initiates the stress response within the body causing blood sugar levels to rise. It is wise to keep this in mind when your health is deteriorating due to no other known factors or when you get a diagnosis for a disease that is a mystery. Setting yourself free from this emotional burden may just be a life saver.... How I maintain a healthy hormonal status.
I am 48 years old and nearing my peri- menopausal stage. My philosophy has always been that if I can maintain a menstrual cycle, my hormones will remain active and “change of life" will be delayed until an appropriate time. So far so good. Mercifully my plan has worked and I remain asymptomatic. This is what I attempt to do. 1. Liver Detoxification. Your liver plays an integral role in detoxifying many toxins and substances including any excess of hormones. Hormones are produced by the body and where there is excess of a hormone, it needs to be eliminated to keep the balance of all the hormones accurate. I take a liver detoxification aid on a daily basis. I combine this with a diet abundant in vegetables from the cruciferous family (cabbage, kale, cauliflower, broccoli, Brussels sprouts) to aid detoxification. 2. Vitamin D. This vitamin is classed as a prohormone. It plays an active role in regulating hormone levels. I keep my levels in the optimal range by taking 5000ius daily 3. Chaste tree. This incredible little berry has the ability to regulate estrogen and progesterone levels and to keep them in the correct ratio of 1:10. A lot of unpleasant hormonal symptoms arises from having a level of estrogen that is too high. Chaste tree will boost progesterone levels in a natural way. I take one tablet daily. 4. Good fats All the hormones in your body is manufactured from good fats that you get from your diet. I make sure that I consume enough good plant fats daily to keep my levels optimal. I include the following good fat sources in my diet: avocados, nuts and seeds, coconut oil and cream, good plant oils like avocado or other nut oils and fish. For assistance with your hormones please contact Naturopathic health care centre on 012 460 9216. Are you struggling to fall pregnant? Disappointed by recurrent miscarriages? Being diagnosed with PCOS? A new programme, Supreme Fertility uses DNA testing to address the root cause of couples struggling to conceive. This, together with a fertility consultation, lifestyle guidance and the right supplementation is helping couples to become the healthiest that they can be in order to fall pregnant naturally.
A staggering 50% of infertility cases are caused by genetic issues which is why, instead of generalised treatment, Supreme Fertility will do DNA tests on couples to find out more about their genetic makeup and ability to conceive. With DNA as a starting point, doctors are swiftly able to identify possible genetic weaknesses and biological challenges and prescribe a course of treatment using this valuable information. Supreme Fertility provides an affordable six-month programme, including DNA testing for both partners with unexplained infertility, PCOS, endometriosis, or with a personal or family history of infertility and/or miscarriages, and when physical causes of infertility have been excluded, or before trying in vitro fertilization (IVF). The ideal time to do this is preconception, to ensure the optimal health of both parents. Supreme Fertility equips patients with an understanding of infertility linked to female factors such as recurrent miscarriages, implantation failure, and the potential genetic causes of these, such as disrupted circadian rhythms, retaining heavy metals, endometriosis, pelvic inflammatory disease, uterine fibroids and more. By providing a list of screenings, one is able to determine if any of these are evident. In this way, further obstacles to falling pregnant are eliminated. For males, genes can shed light on why they may experience low sperm motility, low sperm count, sperm DNA damage or hormonal imbalances. The programme also provides suggested solutions to help manage or overcome these. Supreme Fertility builds on exactly that and enables both the mother and father to improve their health and well-being in order to increase their chances of natural conception. The programme includes lifestyle guidance and supplementation for both potential parents in order to help them conceive. Many over-the-counter vitamins can greatly benefit the process if taken from the onset of trying to conceive. A specific set are recommended. Prenatal vitamins almost always include folic acid, an essential nutrient that helps prevent devastating birth defects. However, what is not so well known is that approximately 50% of individuals’ bodies are unable to convert folic acid into folate, the form needed for it to be effective. Supreme Fertility has launched a folate supplement to address this vital concern. This is merely one example of the solutions proposed by the programme. Because eating is such an important part of equipping the body with the strength to conceive, a recommended eating plan is included for both him and her. This programme not only suggests what to eat, and what not to eat, but also makes recommendations about individual micronutrients (vitamins and minerals) to ensure that the body can redirect this energy. Lifestyle changes such as the use of cell phones, laptops, air filtration, stress levels and an optimal BMI (body mass index) are recommended as part of this unique programme. Additionally, a recommended detoxification of one’s house, food and personal care products as well as what to look out for on labels, are included. And while the adage “self-care” is often used loosely, Supreme Fertility specifies and emphasises the importance of this in specific ways. The Supreme Fertility program is now available through us. Email us on [email protected] to find out more today. Our children are in a state of mental health emergency.
Dr. M de Klerk Even before the pandemic, by the time kids are 18, almost 1 in 2 are diagnosed with any mental health disorder. Even before the pandemic, suicide was the 2nd leading cause of death in our youth ages 10-24 years, only second to unintentional injury, and far above influenza-related deaths. Children 10-14 years old are 13X more likely to die by suicide than influenza & for teens 15-19 that number climbs to 27X. Even during the pandemic, injury & suicide remained the top 2 causes of death among children & teens, and yes - even higher the pediatric deaths from COVID-19. In the winter of 2020, ER visits for suicide attempts by children ages 12-17 jumped almost 40% compared with the pre-pandemic winter of 2019. As we grapple with how this pandemic will end, let’s not forget that the epidemic of childhood anxiety & depression has been raging unchecked. We might think that only adults are burdened by this pandemic, financially and emotionally, but please do not disregard the effect on our children. Just because they can not vocalize their fears and worries like we do, we should not simply glance over their distress. Talk to them, make sure they know that you support them. And love them..... If they need extra support, natural functional medicine offers wonderfull effective treatments to support them on various levels. How to Manage your Anxiety Now
- Green Tea Instead of Coffee L-theanine is an amino acid that promotes a sense of calm and happens to be high in green tea. If you feel more anxious with coffee or between meals, rather stop the coffee and opt for some green tea instead. L-theanine is typically taken at 200 mg twice daily in supplement form. - Taurine Taurine is a precursor to GABA, an inhibitory neurotransmitter that most people with anxiety are low in. The general starting dose is about 500 mg daily. - Passiflora Passiflora encourages healthy levels of GABA and can help ease anxiety. It is very useful to carry with you, and when you feel the anxiety bubbling up, take a recommended dosage. - Practice your deep breathing Whenever you feel overwhelmed, take 5 deep breaths. This will reset your active stressed nervous system into a more peaceful state. Try and do this several times a day to prevent you from getting to a full on panicked state Healing anxiety and depression through functional medicine removes the need for pharmaceutical management of your mood. Finding and treating the root cause can take time, but hopefully your practitioner can investigate and find the cause and put you on the path to healing. If you need any help with your anxiety or depression, please do not hesitate to contact us. Dr. M de Klerk Nutritional deficiencies might contribute or even be the cause of your depression and anxiety.11/25/2021 Nutritional deficiencies might contribute or even be the cause of your depression and anxiety.
Dr. M de Klerk Nutrient deficiencies are a lot more common than you might think. If you have a digestive tract that does not work properly, your ability to absorb nutrients will be less and you will become deficient quicker. Being on a restrictive diet of any kind for too long, for example veganism, vegetarianism, keto, or autoimmune protocol, can put you at risk for deficiencies. Having a varied diet from all the food groups is essential. If you’re taking a nutrient depleting medication like the birth control pill, places you at an increased risk for nutrient deficiencies. Medication that block acid, like PPIs and Tums, as well as those used in diabetics can create nutrient deficiencies that can manifest as anxiety and depression as well. Nutrients like omega-3 fatty acids, EPA and DHA, B6, Inositol, folate, B12, copper, zinc, magnesium, and vitamin D have a direct impact on mood and are common deficiencies in people. Additionally, if you have any issues with protein absorption you will be deficient in the amino acids your body needs to make neurotransmitters. How to Heal Nutrient Deficiencies Have Appropriate Lab Testing The following blood tests will give you indication of what you are deficient in: • CBC • Ferritin • Vitamin D • Magnesium • B12 • Folate • Homocysteine • And others as needed Adopt a Whole Foods Diet On top of optimizing gut health and absorption, you’ll also need to focus on a nutrient dense diet. Eat colorful, fresh foods in abundance. In my next article I will discuss ways that you can improve your depression and anxiety in the interim while your practitioner works on identifying the root cause. Nutrient Deficiencies
Dr. M de Klerk Nutrient deficiencies are a lot more common than you might think. If you have a digestive tract that does not work properly, your ability to absorb nutrients will be less and you will become deficient quicker. Being on a restrictive diet of any kind for too long, for example veganism, vegetarianism, keto, or autoimmune protocol, can put you at risk for deficiencies. Having a varied diet from all the food groups is essential. If you’re taking a nutrient depleting medication like the birth control pill, places you at an increased risk for nutrient deficiencies. Medication that block acid, like PPIs and Tums, as well as those used in diabetics can create nutrient deficiencies that can manifest as anxiety and depression as well. Nutrients like omega-3 fatty acids, EPA and DHA, B6, Inositol, folate, B12, copper, zinc, magnesium, and vitamin D have a direct impact on mood and are common deficiencies in people. Additionally, if you have any issues with protein absorption you will be deficient in the amino acids your body needs to make neurotransmitters. How to Heal Nutrient Deficiencies Have Appropriate Lab Testing The following blood tests will give you indication of what you are deficient in: • CBC • Ferritin • Vitamin D • Magnesium • B12 • Folate • Homocysteine • And others as needed Adopt a Whole Foods Diet On top of optimizing gut health and absorption, you’ll also need to focus on a nutrient dense diet. Eat colorful, fresh foods in abundance. Gut Health & ANXIETY
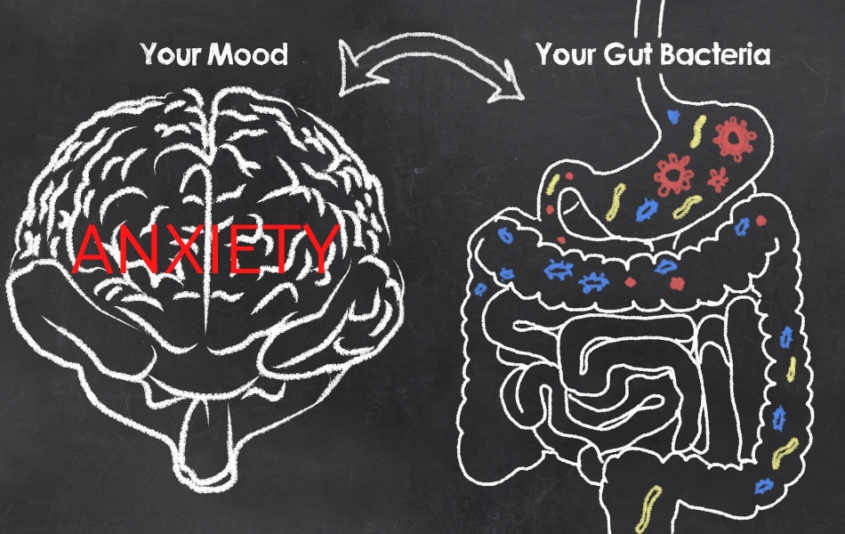
by M de Klerk “Fire in the gut means fire in the brain.” Or in other words, if your gut is inflamed then your brain will be definitely too. Infections like SIBO, bacterial dysbiosis, parasites, yeast overgrowth, and H. pylori can be one cause of inflammation. Leaky gut and food sensitivities can also be a source of inflammation. As you can imagine, having brain inflammation makes us irritable, angry and anti-social. All your calm and happy inducing neurotransmitters are also decreased, leaving you to feel anxious and depressed. Your Gut Makes Serotonin About 400 times more serotonin is found in your gut than your brain to be exact. WOW! So it would appear that your gut may be the main centre of neurotransmitter synthesis and not your brain. Which makes sense why when you heal someone’s gut their mood gets better. How to Heal Your Gut? 1. Have Lab Testing Completed Having some labs done for your Gut could be beneficial. Your health care practitioner will be able to guide you here. 2. Removing Stressors Identify and remove any stressors that could be contributing to poor gut health. Here are two big areas to start with. 3. Unnecessary Medications. Remove NSAIDs, proton pump inhibitors (PPIs), unnecessary antibiotics, and birth control. Talk with your doctor before discontinuing meds. 4. Life Stressors. Like we mentioned above, chronic stress can actually change the makeup of your microbiome. It also disrupts the HPA-axis (hypothalamic-pituitary-adrenal), which affects pretty much all the hormones in your body. 5. Food stressors Remove foods from your diet that is know to cause irritation and inflammation in your intestines. Most people are sensitive to wheat, dairy, sugar and soya. Add Fermented Vegetables and fibre to your diet. This is a great way to begin getting some beneficial bacteria going in your gut! Raw, cultured, organic vegetables like pickles, sauerkraut, and other fermented vegetables like beets and carrots can promote the growth of good bacteria in the gut. In the case of SIBO or yeast overgrowth, we avoid these foods until infection is resolved. Your doctor will be able to guide you here. Bacteria need food to grow and thrive. Vegetables contain lots of fibre and will promote healthy growth. Image Source: motherhoodcommunity.com /the-gut-brain-connection OCTOBER is MENTAL HEALTH AWARENESS MONTH
by Dr. M de Klerk Anxiety is so common that I am sure that you know someone who has had or currently has anxiety. Perhaps you are suffering from anxiety and you are trying to understand why this has happened to you. You are probably also exploring different options to make your anxiety better. The conventional perspective on anxiety is perhaps too simplified —myou have a neurotransmitter imbalance and you need a medication to re-establish that balance. This treatment may work, but not always. This assumes that you are broken and the only fix is a pharmaceutical drug that you might have to take for many years. And if you’ve chosen a medication to manage your symptoms—you have done nothing wrong. In my next article I would like to offer you some tools to help you manage your symptoms…and maybe even kick the anxiety for good. |
AuthorsDr. Marike de Klerk Categories
All
|
All rights reserved Naturopathic Health Care Centre
ADDRESS: No 13 Hazelwood Road, Hazelwood, Pretoria
TELEPHONE: 012 460 9216
PAIA Manua
Website design and digital marketing by Plan Me Pretty (PTY) Ltd
TELEPHONE: 012 460 9216
PAIA Manua
Website design and digital marketing by Plan Me Pretty (PTY) Ltd












 RSS Feed
RSS Feed